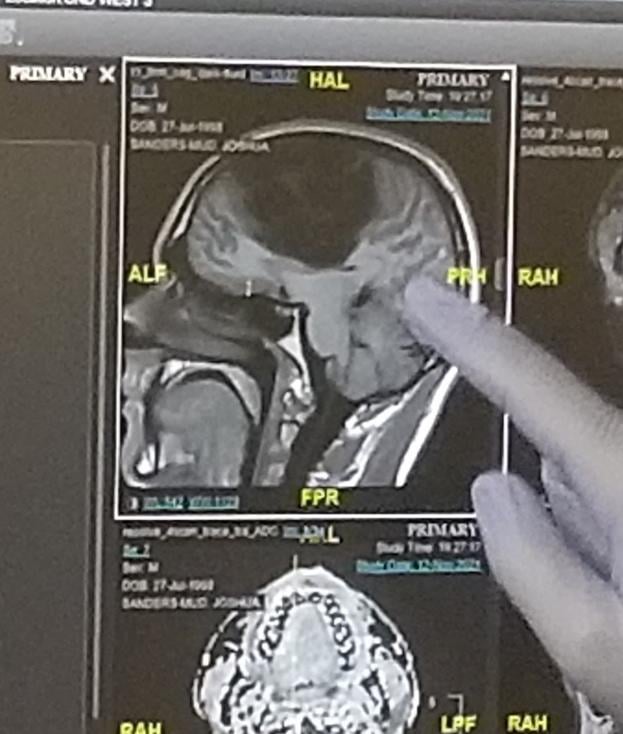
Over a third of my brain was removed
Living Beyond Limits: Understanding Life After Major Brain Surgery
Imagine undergoing a surgery that removes over one-third of your brain. For most, this sounds like science fiction—yet for thousands of people worldwide, it’s a life-saving reality. Procedures like hemispherectomies (removal of one brain hemisphere) or large-scale lobectomies (removal of a brain lobe) are performed to treat severe neurological conditions, offering patients a chance at a functional life. But what happens next? This article explores the science, recovery, and resilience behind living with significantly altered brain anatomy.
Why Remove Part of the Brain?
Brain resection surgeries are typically last-resort treatments for debilitating conditions unresponsive to medication or other therapies. Common reasons include:
- Severe Epilepsy: When seizures originate in a specific, damaged brain region and threaten quality of life.
- Brain Tumors: To remove malignant or benign growths impacting critical functions.
- Traumatic Injury: To alleviate pressure or repair damage after accidents.
- Rasmussen’s Encephalitis: A rare inflammatory disease causing progressive brain damage.
In cases like pediatric epilepsy, removing 35–40% of the brain (e.g., an entire hemisphere) can drastically reduce seizures. The brain’s adaptability, especially in children, often compensates for lost tissue.
The Surgery: Precision and Risk
Hemispherectomies and large resections are complex, high-stakes procedures. Surgeons meticulously disconnect affected areas while preserving blood flow and minimizing damage to healthy tissue. Two primary approaches exist:
- Anatomical Hemispherectomy: Removal of the entire hemisphere.
- Functional Hemispherectomy: Disconnecting the hemisphere but leaving it in place.
Risks include infection, bleeding, and temporary or permanent neurological deficits. However, success rates are promising—studies show 60–80% of epilepsy patients become seizure-free post-surgery.
Recovery: The Brain’s Remarkable Plasticity
The most astonishing aspect of recovery is neuroplasticity—the brain’s ability to rewire itself. When a large portion is removed, remaining regions gradually take over lost functions:
- Children’s brains adapt most dramatically, often relearning language, motor skills, and cognition.
- Adults may require intensive rehabilitation but can still regain significant abilities.
For example, if the left hemisphere (responsible for language in most right-handed people) is removed, the right hemisphere may compensate, allowing speech recovery.
Key Rehabilitation Tools:
- Physical & Occupational Therapy: Rebuild motor skills.
- Speech Therapy: Restore communication.
- Cognitive Behavioral Therapy (CBT): Address emotional challenges.
Long-Term Outcomes: What to Expect
Life after major brain surgery varies widely. Factors like age, pre-surgery health, and rehabilitation commitment play critical roles:
- Seizure Control: Most patients experience fewer or no seizures.
- Mobility: Weakness on one side of the body (hemiparesis) is common but manageable with aids like braces.
- Cognitive Function: Some memory or attention challenges may arise, though many return to school or work.
- Emotional Health: Depression or anxiety can occur due to trauma, but support networks improve outcomes.
Case Study: At 6 years old, Sophie underwent a hemispherectomy for Rasmussen’s encephalitis. Now a teenager, she walks, talks, and attends mainstream school—proof of her brain’s resilience.
Debunking Myths: “Will I Still Be Myself?”
A common fear is that removing brain tissue alters personality or identity. However, personality arises from complex neural networks, not localized regions. Most patients retain their core identity, with emotional shifts often linked to recovery stress rather than the surgery itself.
The Future of Brain Recovery
Advances in neurotechnology—from AI-powered prosthetics to stem cell therapies—promise even better outcomes. Research in brain-computer interfaces (BCIs) could someday restore lost functions entirely.
Conclusion: Redefining Resilience
Removing a third of the brain isn’t a death sentence—it’s a testament to medical innovation and human tenacity. While challenges remain, most patients regain independence and embrace fulfilling lives. If you or a loved one faces this journey, seek support from specialized neurology teams and patient communities.
Key Takeaways:
- Brain resection treats severe epilepsy, tumors, or injury.
- Neuroplasticity empowers recovery, especially in children.
- Rehabilitation is critical for maximizing outcomes.
- You’re more than your anatomy—resilience defines the human spirit.
For More Information:
- Epilepsy Foundation: Resources on surgical options.
- Johns Hopkins Pediatric Neurosurgery: Leading experts in hemispherectomy.
- Brain Recovery Project: Support for families post-surgery.
Have questions or a story to share? Comment below or reach out to neurology specialists near you.